Skin Conditions of the
Cavalier King Charles Spaniel
-
 List
of Disorders
List
of Disorders - Symptoms
- Diagnosis
- Treatment
- Veterinary Specialists
- Research News
- Related Links
- Veterinary Resources
Cavalier King Charles spaniels have been reported to be pre-disposed to certain conditions affecting their skin. We list here those which have been identified and described in published veterinary literature.
We do not include all skin conditions common to many breeds, but only those specifically reported as especially affecting CKCSs.
List of Disorders
Skin conditions reported in the cavalier King Charles spaniel breed include:
- Alopecia areata
- Black hair follicular dysplasia
- Canine atopic dermatitis (atophy)
- Copper associated hepatopahty (CAH)
- Curly Coat / Rough Coat syndrome
- Cyclosporine-induced dermatosis
- Dermoid sinus
- Malassezia dermatitis
- Mange
- Necrolytic dermatitis
- Pemphigus foliaceus
- Piebaldism
- Sebaceous adenitis
- Skin cancers
- Staphylococcus intermedius
Alopecia areata
 Alopecia
areata (AA) is an immune system disfunction which attacks the dog's hair
follicles, causing hair loss, usually in patches. “Alopecia” is the
medical term for hair loss, and “areata” means that it occurs in small,
random areas. In dogs, it may be associated with diabetes or thyroid
disease. AA is not curable, but medications and other treatments help
manage the hair loss, and while treated, hair may regrow. Treatments
usually include corticosteroids, immunotherapies, and phototherapy.
Alopecia
areata (AA) is an immune system disfunction which attacks the dog's hair
follicles, causing hair loss, usually in patches. “Alopecia” is the
medical term for hair loss, and “areata” means that it occurs in small,
random areas. In dogs, it may be associated with diabetes or thyroid
disease. AA is not curable, but medications and other treatments help
manage the hair loss, and while treated, hair may regrow. Treatments
usually include corticosteroids, immunotherapies, and phototherapy.
In this October 2024 article, a cavalier was diagnosed with both alopecia areata and a disorder of the eyes, uveodermatological syndrome (CUDS). CUDS is an autoimmune disease which affects both the eyes and patches of skin. See our Eyes webpage for a discussion of uveodermatological syndrome.
RETURN TO TOP
Black hair follicular dysplasia
Black hair follicular dysplasia is an uncommon cause of hair loss in the black colored regions of the dog's coat. The loss begins as early as one month after birth and progresses to the point that all black hair may be lost by 8 to 9 months of age. Less severe cases display a dull coat or wooly coat in the black areas, abnormal hair growth, dry skin, and/or scally skin. In a December 1995 article, UK clinicians report that a 3 year old tricolored female cavalier King Charles spaniel had a "poor fluffy haircoat affecting only dark haired areas."
According to Muller and Kirk's Small Animal Dermatology, black hair follicular dysplasia has been recognized in many breeds, including cavaliers. Dogs are born normal but show coat changes by 4 weeks of age. Only the black hairs are affected. The first noticeable change in most dogs is loss of luster of the black hairs, followed by progressive hair loss until all black hairs are lost.
RETURN TO TOP
Canine atopic dermatitis (atophy)
 Canine atopic dermatitis
(CAD), or atophy, is due to an inherited tendency to develop
IgE antibodies in response to exposure to allergens that
are inhaled or absorbed through the skin.
Canine atopic dermatitis
(CAD), or atophy, is due to an inherited tendency to develop
IgE antibodies in response to exposure to allergens that
are inhaled or absorbed through the skin.
In a December 2016 article, a team of University of California-Davis reasearchers examined the medical records from 1995 to 2010 of 90,090 dogs of all AKC-recognized breeds treated at their veterinary hospital, to determine the relation between neuter status and autoimmune diseases. They report finding that neutered dogs had a significantly greater risk of atopic dermatitis.
RETURN TO TOP
Copper associated hepatopahty (CAH)
The cavalier breed has been found to be predisposed to copper associated hepatopahty (CAH). CAH describes excessive quantities of the metal copper (Cu) in the dog's liver. Copper normally is processed by the liver into bile by certain proteins. When the dog's liver is unable to convert copper, it accumulates in the liver and causes inflammation, scarring of the liver, and death of liver cells. Symptoms of CAH rarely are evident before permanent damage to the liver's cells occur.
CAH is discussed at greater length on our Liver Disorders webpage.
RETURN TO TOP
Curly Coat / Rough Coat syndrome
Curly coat syndrome is a severe congenital condition of the skin, coat, claws, and eyes in some cavalier King Charles spaniel puppies. It is also known as rough coat syndrome and its scientific name is ichthyosis keratoconjunctivitis sicca and also as congenital keratoconjunctivitis sicca and ichthyosiform dermatosis (CKCSID).
Curly coat syndrome is discussed at greater length on our Curly Coat webpage.
RETURN TO TOP
Cyclosporine-induced dermatosis
Cyclosporine (ciclosporin) is a calcineurin inhibitor which is used to treat chronic canine atopic dermatitis (CAD) and also various immune-mediated and inflammatory diseases. A rare side effect of this drug are skin disorders such as thickening of the gums (gingival thickening), thickening of the paw pads (hyperkeratosis), lumpy growths on the skin (papillomatosis), and other skin lesions. One of them is called psoriasiform-lichenoid dermatosis, which is more common among English springer spaniels than any other breed. It is an inflammatory skin disease causing itchiness.
In an August 2024 article, a team of Japanese clinicians reported case studies of 4 dogs diagnosed with psoriasiform-lichenoid dermatosis associated with treatment for several months with cyclosporine for immune-mediated diseases. One of these dogs was a 7 year old cavalier being given oral cyclosporine and pednisolone (for polyarthritis) for 7 months. The cavalier developed chronic eczema with lichenoid plaques, scales, and hyperpigmentation, and hair loss around its eyes, mouth, and abdomen after 5 months of treatment. At that point, the prednisolone was discontinued, but the dermatitis continued. The clinicians treated the cavalier with amoxicillin, a penicillin antibiotic used to treat bacterial infections for a week, and bathed with a salicylic acid shampoo and moisturizer, all with no improvement. They then reduced the dosage of cyclosporine by half (from 17.5 to 8.8 mg/kg/day). Three weeks later, hair began to grow again around the mouth and body. After 8 weeks, the lichenoid plaques, scales and hyperpigmentation had almost disappeared. The dog died 3.5 months later due to an unspecified unrelated cause. He was diagnosed with psoriasiform-lichenoid dermatosis accompanied by cocci proliferation and infection, induced by cyclosporine. The clinicians concluded that psoriasiform-lichenoid dermatosis may develop in dogs receiving high dosage or long-term administration of cyclosporine.
RETURN TO TOP
Dermoid sinus
 Dermoid sinus* is a congenital
skin defect caused by the failure of the skin to separate from the
ectodermal neural tube of the nervous system during development of the
embryo of the dog. Among dogs, it occurs most often along the midline
back of Rhodesian ridgebacks. It is in the form of a tubular sac that
extends from the skin to underlying tissues. There are five types of
dermoid sinuses, Types !, II, III, IV, and V. based upon the formation
of the sinus.
Dermoid sinus* is a congenital
skin defect caused by the failure of the skin to separate from the
ectodermal neural tube of the nervous system during development of the
embryo of the dog. Among dogs, it occurs most often along the midline
back of Rhodesian ridgebacks. It is in the form of a tubular sac that
extends from the skin to underlying tissues. There are five types of
dermoid sinuses, Types !, II, III, IV, and V. based upon the formation
of the sinus.
In a December 2023 article, UK clinicians reported a Type IVb dermoid sinus attached to the dura matter of the brain, located between the eyes of a cavalier at the midline of the frontal bones of the skull. It drained fluid through a lesion in the skin. (See photo.) The sinus was removed in a surgical procedure, which incuded a synthetic graft of the dura matter over the frontal lobes.
* Dermoid sinus is also called a dermoid cyst and a pilonidal sinus.
RETURN TO TOP
Malassezia dermatitis
Malassezia dermatitis (malassezia pachydermatis) consists of yeast infections, for which the CKCS has been found to be at increased risk. See these veterinary reports for details about this disorder in cavaliers.
RETURN TO TOP
Mange
Mange comprises a variety of skin diseases caused by mites. Mites are very small parasitic insects, much smaller than either ticks or fleas, and often seemingly invisible. Three types of mange commonly affect dogs, each caused by different types of mites.
Cheyletiellosis
 Cheyletiellosis
(Cheyletiella dermatitis; walking dandruff) is a highly contagious skin
disorder (dermatosis) caused by an infestation of the surface-dwelling
Cheyletiella spp, a parasitic mite. They live in the outer layer of the
dog's (and human's) skin and feed on surface debris and tissue fluids.
The females shed eggs into the host animal's hair. They are highly
contagious. The primary symptoms are itching, scaling mainly on the
dog's back, and redness of the skin.
Cheyletiellosis
(Cheyletiella dermatitis; walking dandruff) is a highly contagious skin
disorder (dermatosis) caused by an infestation of the surface-dwelling
Cheyletiella spp, a parasitic mite. They live in the outer layer of the
dog's (and human's) skin and feed on surface debris and tissue fluids.
The females shed eggs into the host animal's hair. They are highly
contagious. The primary symptoms are itching, scaling mainly on the
dog's back, and redness of the skin.
Cheyletiella are large, saddle-shaped mites, whitish in color, visible to the eye, and tend to move rapidly. They have appendages called palps which look like legs with claws on their ends near their mouths, and they have legs with rows of hair.
Cheyletiellosis is diagnosed by their visible appearance, plus brushing the dog’s coat and scraping the skin, collecting the mites and their refuse, and examining the scrapings under a microscope or just a magnifying glass, looking for their familiar shaped bodies.
In a November 2000 article, Vienna, Austria veterinary dermatologists diagnosed Cheyletiella dermatitis on the back of a cavalier King Charles spaniel (above, right) with a two-month long history of excessive itching. They observed white scales on the dog's back, although the skin looked normal. Microscopic examination showed live mites and their eggs. The dog's owner also was infested, with her legs and abdomen covered with itchy red bumps. The cavalier was treated first with dips of Bayer's phoxim (Baythion, Baymite, Sebacil, Valexone) a highly toxic organophosphate insecticide available to veterinarians in Europe. Since the dog continued itch somewhat, she then was treated with moxidectin (Advantage Multi, ProHeart). The signs and itching eventually disappeared.
See also this December 2002 article, which concludes that selamectin (Revolution, Paradyne, Stronghold, Chanhold) successfully treated cheyletiellosis in a family of nine cavaliers.
Demodectic mange
 Demodectic
mange (demodicosis, demodex, red mange) is the most common form, caused
by demodectic mites (Demodex canis), a cigar-shaped mite. They
tend to exist on almost all dogs, located in hair follicles and
sebaceous glands, and rarely cause any health problems, unless the
affected dog has a weakened or suppressed immune system. In that case,
they can get out of control, causing patches of hair loss and red,
scaling skin. In extreme cases, the dog’s entire body may be affected
with infections, swelled skin, scaling, and crusting skin. Puppies,
particularly between the ages of 3 and 6 months, are most susceptible to
demodectic mange because their immune systems are not yet fully
developed.
Demodectic
mange (demodicosis, demodex, red mange) is the most common form, caused
by demodectic mites (Demodex canis), a cigar-shaped mite. They
tend to exist on almost all dogs, located in hair follicles and
sebaceous glands, and rarely cause any health problems, unless the
affected dog has a weakened or suppressed immune system. In that case,
they can get out of control, causing patches of hair loss and red,
scaling skin. In extreme cases, the dog’s entire body may be affected
with infections, swelled skin, scaling, and crusting skin. Puppies,
particularly between the ages of 3 and 6 months, are most susceptible to
demodectic mange because their immune systems are not yet fully
developed.
Demodectic mange is diagnosed by scraping the dog’s skin, collecting the mites and their refuse, and examining the scrapings under a microscope, looking for their familiar cigar shaped bodies. (See image of mites on head of a cavalier, above, right).
Supplements: The nutrients allicin and alliin in garlic has been shown to kill microorganisms on contact. Garlic powder lightly sprinkled on food or a clove of garlic, raw or cooked on the food, at the rate of a clove per 10 lbs. of body weight.
Sarcoptic mange
Sarcoptic mange (scabies) is caused by an eight-legged, circular-shaped mite (Sarcoptes scabiei). It is very contagious and can pass from dogs to humans. The female mite burrows into the dog’s skin and lays eggs. Within 3 weeks, the hatched mites feed on the dog’s skin. This mite is not associated with a weak or suppressed immune system.
Symptoms may develop even before the eggs hatch. They may include extreme itchiness, redness, rashes, hair loss, crusty skin, and infections.
Sarcoptic mange is diagnosed by scraping the dog’s skin, collecting the mites and their refuse, and examining the scrapings under a microscope, looking for their familiar round shaped bodies and legs. Since they are so small, it is possible that no mites will appear in the scrapings, and the diagnosis would be made mainly by the severity of the symptoms.
Treatment
The conventional treatment for mites is a topical application of selamectin or imidacloprid-moxidectin. The nutrients allicin and alliin in garlic has been shown to kill microorganisms on contact. Garlic powder lightly sprinkled on food or a clove of garlic, raw or cooked on the food, at the rate of a clove per 10 lbs. of body weight.
RETURN TO TOP
Necrolytic dermatitis
 Superficial necrolytic dermatitis (SND) typically appears as
thickened, crusting, ulcerative lesions on the dogs' paw pads, but also
may appear at other pressure points. such as elbows, and at
mucus-to-skin boundaries, such as the nose and lips, anal, and/or
genital regions. It is a form of hyperkeratosis.
Superficial necrolytic dermatitis (SND) typically appears as
thickened, crusting, ulcerative lesions on the dogs' paw pads, but also
may appear at other pressure points. such as elbows, and at
mucus-to-skin boundaries, such as the nose and lips, anal, and/or
genital regions. It is a form of hyperkeratosis.
It most often is associated with a liver disorder, hepatocutaneous syndrome (HCS), in which severe lesions appear as nodules on the surface of the liver. HCS is a progressive disorder which usually is fatal. Therefore, treatment focuses upon the liver aspects of this disorder. See our Liver Disorders webpage for more information about this combination of disorders. See also this January 2023 article.
RETURN TO TOP
Pemphigus foliaceus
 Pemphigus foliaceus (PF) is an autoimmune skin disease, in which the
body’s immune system attacks the connections between the layers of skin
cells. The affected dog's immune system incorrectly recognizes a
component of skin, desmocollin-1, a component of desmosomes, as being a
foreign invader and then produces antibodies which bind to the the
desmosomes and destroy them. The destruction causes the outer layer of
skin to split and fill with fluid, leading to pustules and blisters,
which rupture, typically resulting in hair loss, scabs, and ulcers. It
is the most common autoimmune skin disease in dogs, most often observed
in middle-aged and older dogs.
Pemphigus foliaceus (PF) is an autoimmune skin disease, in which the
body’s immune system attacks the connections between the layers of skin
cells. The affected dog's immune system incorrectly recognizes a
component of skin, desmocollin-1, a component of desmosomes, as being a
foreign invader and then produces antibodies which bind to the the
desmosomes and destroy them. The destruction causes the outer layer of
skin to split and fill with fluid, leading to pustules and blisters,
which rupture, typically resulting in hair loss, scabs, and ulcers. It
is the most common autoimmune skin disease in dogs, most often observed
in middle-aged and older dogs.
In a September 2019 article, a team of Colorado State veterinary researchers report the case of a 9 year old castrated male cavalier with a 6 month history of pruritus and crusting, affecting the paw pads, claw folds, prepuce, scrotum, ear leathers, and muzzle. Pemphigus foliaceus was confirmed by a biopsy. The cavalier had been treated unsuccessfully with prednisolone and mycophenolate, also resulting in muscle wasting and other unwanted side effects. Polysulfated glycosaminoglycan (PSGAG) then was injected under the skin for four days, along with oral doses of prednisolone and cyclosporine. After four months, the PSGAG treatments resulted in healing of the lesions after 40 days. PSGAG injections were reduced to one a week, and reduced doses of prednisolone and cyclosporine continued. Within two weeks, the PF recurred, and treatments were increased. After two injections of PSGAG, the lesions healed. Six months later, crusting appeared again on the muzzle, scrotum, and paws. Treatment frequencies were increased, and within two months the crusting healed. Frequency of treatment with prednisolone then was decreased but the dog continued to be treated with cyclosporine at the same rate. No further signs of PF were present after a total of 21 months of treatments. [See photo at right of the patient before treatment with PSGAG.]
RETURN TO TOP
Piebaldism
Piebaldism is a benign genetic disease caused by a mutation which
results in the patches of fur which lack pigment.
 It
is one of a series of defects called "neurocristopathies", some of which
result as cancer of the nervous system, deafness, digestive problems, or
holes in the heart, which are caused by cells not moving to the right
place as an embryo develops. Piebaldism is caused by a mutation in a
gene called Kit.
It
is one of a series of defects called "neurocristopathies", some of which
result as cancer of the nervous system, deafness, digestive problems, or
holes in the heart, which are caused by cells not moving to the right
place as an embryo develops. Piebaldism is caused by a mutation in a
gene called Kit.
The mutation causes melanocytes cells in the early embryo to fail to migrate correctly. Melanocytes are responsible for pigmentation of hair and of skin. These cells start at the back of the embryo and they try to migrate around through the skin and cover the whole of the embryo's skin. When arkly colored pigment cells do not proliferate enough -- not making enough daughter cells to colonize or cover the whole region of the skin that needs to be covered by the time the pigmentation pattern is set down -- regions of skin or hair result in lacking pigment, usually at the front of an animal.
In particular, regarding the association of piebaldism and deafness, cavaliers are potentially subject to pigment-associated congenital sensorineural deafness, which should be evident in the puppy age span. See our deafness webpage for more information.
In a March 2017 article, the investigators include a photo of a cavalier with axial depigmentation, a form of piebaldism. See photo at right.
RETURN TO TOP
Sebaceous adenitis
Sebaceous adenitis is an inflammatory reaction which damages the sebaceous glands of the skin. The sebaceous glands produce an oily secretion called sebum, which serves in part to hydrate the skin, particularly in haired areas. Sebaceous adenitis causes the dog's coat of hair to become dry and brittle. It has been identified in the cavalier and a few other breeds, particularly spaniels.
RETURN TO TOP
Skin cancers
Cancers of the skin include carcinoma, mastocytoma, lymphoma, mast cell tumors, and melanoma. All of these cancers are discussed at greater length on our Cancer webpage.
Staphylococcus intermedius
Staphylococcus intermedius is regarded as the primary bacteria which infects the skin in dogs. It causes a pus (pyoderma) reaction on the skin. It has been reported in cavalier King Charles spaniels, and in an October 2003 article, it was found to have been transferred from cavalier bitches to their puppies immediately after birth.
RETURN TO TOP
Symptoms
Several of these skin disorders have common clinical signs, particularly the crusting or scaling of the skin. Scaling consists of flaking loose skin. Crusting is an accumulation of several different things, such as dried serum, pus, exudate, blood, bacteria, and yeasts. Pus on the skin is called pyoderma.
Itchiness is called pruritis, and while not all of the disoders listed here cause itchiness, several of them do. Pruritus is measured using any of a variety of scales, all involving collecting observations from the dogs' owners.
More severe symptoms include openings through the skin surface through which fluids discharge. These may be draining tracks or ulcers and lesions.
RETURN TO TOP
Diagnosis
Because so many different skin disorders have the common clinical sign of the crusting or scaling of the skin, crusting is not a diagnosis or even specific for certain conditions. Since the external appearance of the skin is only symptom and not the disease itself, thorough general and dermatological examinations of the dog need to be performed to diagnose the underlying disease.
Hair, saliva, and/or serum testing were not reliable at diagnosing specific food reactions in dogs. Elimination diets have been found to be effective in identifying food reactions. However, food allergies are only one of several possible underlying causes of skin disorders.
Thorough physical examinations by holistic veterinarians often detect the most likely underlying causes of skin eruptions and itchiness. Causes may be totally unrelated to environmental conditions. They may be due to internal organ disorders, such as the liver.
RETURN TO TOP
Treatment
The courses of treatment will depend upon the specific diagnoses. However, the most common initial treatments of itchiness and rashes are efforts to mask the itchiness and rashes. The treatments may be topical, such as ointments, or internal, but they are not intended to affect the underlying cause of the symptoms -- only to stop them from continuing to occur.
Medicines
Glucocorticoids, including triamcinolone acetonide (Vetalog, Kenalog, Cortalone, TriamTabs, Aristocort), which is an anti-inflammatory and immune suppressant.
Oclacitinib (Apoquel), a novel Janus kinase (JAK)
inhibitor, has been approved for the control and treatment of atopic
dermatitis (AD) in dogs 12 months of age or older. Kinases are signaling
compounds that cells use to communicate with each other. JAKs play major
roles in dogs' growth and development, including
 forming
red and white blood cells from bone marrow stem cells, regulating
inflammatory response, maintaining antibody-producing cells, and
controlling tumor formation.
forming
red and white blood cells from bone marrow stem cells, regulating
inflammatory response, maintaining antibody-producing cells, and
controlling tumor formation.
In a June 2015 article, oclacitinib has been shown to be "safe and efficacious for long-term use and improved quality of life in the 247 dogs in the study, including cavaliers. This study was sponsored by Zoetis, the maker of Apoquel. In a June 2023 article, USA specialists concluded that, "Oclacitinib has proven to be a great tool in our armamentarium and has opened countless opportunities for an alternative option to the use of glucocorticoids." See, also, this May 2024 article.
Reported adverse reactions to this drug include:
• itching
• dermatitis
• skin infections
• hair loss
• vomiting
• diarrhea
• urinary incontinence
• neurologic disorders
• behavior changes
• lethargy
• excitability
• seizures
• convulsions
• auto-immune disease (IMHA)
• blood clotting disorders
• liver disorders.
The maker of Apoquel provides this "Important Safety Information" about the drug: "Do not use APOQUEL in dogs less than 12 months of age or those with serious infections. APOQUEL may increase the chances of developing serious infections, and may cause existing parasitic skin infestations or pre-existing cancers to get worse.”
In a
March 2024 article, a study involving 22 dogs (11 PUFA and 11
placebo) diagnosed with nonseasonal environmentally induced cAD, the
researchers report finding that daily doses of fish oil --
polyunsaturated fatty acids (PUFA) -- allowed for the reduction of
dosage of oclacitinib and improved the dogs' pruritus
Visual Analog
Scale (PVAS), quality of life, and Global Assessment (GA) after 16
weeks.
Lokivetmab (Cytopoint) is a mouse-produced antibody
that is licensed in the UK for treating CAD, also manufactured by
Zoetis. Cytopoint is an antibody that binds to and inactivates the
cytokine, Interleukin 31 (IL
 31),
which is part of the dog’s immune system and which prompts the
itch sensation in the brain. Zoetis claims that Cytopoint is more fast
acting than oclacitinib, and has a better safety record, and that it has been found to be as
effective as cyclosporin for dealing with pruritis and inflammation
associated with CAD. There is reason to believe that these claims are
false, with respect to some dogs. It is injected under the skin with follow up
injections no sooner than once a month. See this
May 2024
article.
31),
which is part of the dog’s immune system and which prompts the
itch sensation in the brain. Zoetis claims that Cytopoint is more fast
acting than oclacitinib, and has a better safety record, and that it has been found to be as
effective as cyclosporin for dealing with pruritis and inflammation
associated with CAD. There is reason to believe that these claims are
false, with respect to some dogs. It is injected under the skin with follow up
injections no sooner than once a month. See this
May 2024
article.
Zenrelia (ilunocitinib), an immunomodulator, has been approved by the U.S. Food & Drug Administration (FDA) to control pruritus (itchiness) associated with allergic dermitit in dogs at least a year old. Zenrelia is a synthetic Janus kinase (JAK) inhibitor designed to disrupt cytokine signaling pathways that trigger itch and inflammation related to canine allergic and atopic dermatitis. The most common adverse reactions aere vomiting, diarrhea, and lethargy. This drug has not been evaluated in dogs that are being bred. Also, use of this drug along with glucocoticoids,cyclosporine, or other systemic immunosuppressive drugs has not been tested. Because Zenrelia is designed to suppress the dog's immune system, it reportedly may increase the canine patient's susceptibility to certain infections and neoplasticc conditions, both benign and malignant.
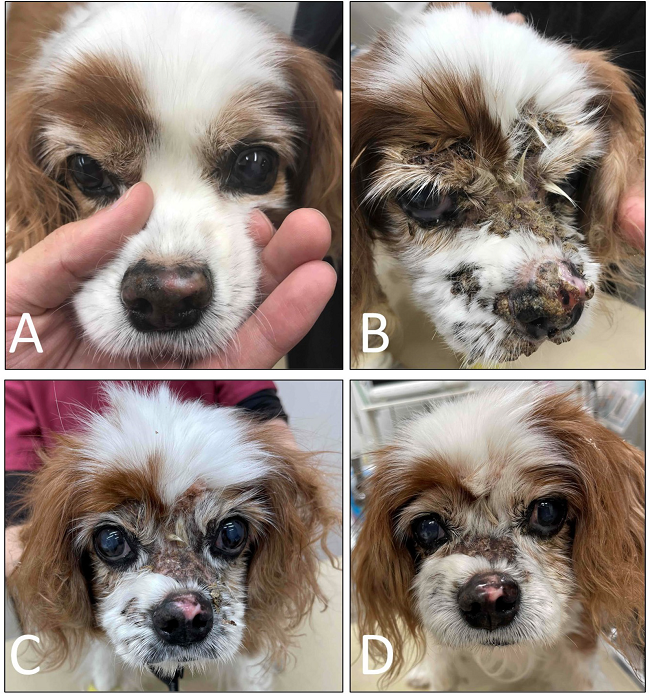
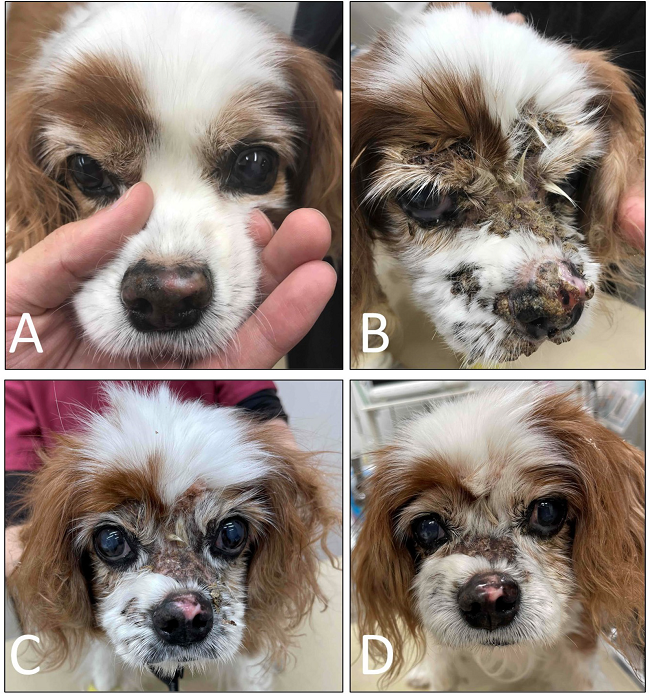
In a January 2022 article, Japanese clinicians reported the successful treatment of a 13-year-old cavalier diagnosed with cutaneous epitheliotropic lymphoma (CEL) resulting in severe facial pruritus, alopecia, erythema, erosion, and ulceration with crust. Once treatments with other medications, including prednisolone, were unsuccessful, lokivetmab was injected periodically. The lokivetmab decreased pruritus. (See photos below.) The authors concluded that anti-IL-31 therapy appears to be a potential treatment option in controlling pruritus associated with CEL in dogs.
 (A)
(A) On Day 14, nasal depigmentation had emerged. (B) On Day 105,
progression of facial alopecia with crusting was found. (C) On Day
132, facial alopecia with crusting was still present. (D) On Day
160, hair regrew on the face where alopecia was present.
(A)
(A) On Day 14, nasal depigmentation had emerged. (B) On Day 105,
progression of facial alopecia with crusting was found. (C) On Day
132, facial alopecia with crusting was still present. (D) On Day
160, hair regrew on the face where alopecia was present.
RETURN TO TOP
Alternatives
These alternative treatments to prescription medicine are faried in type and effectiveness. Apart from fecal microbiota transplantations, very little scientific research, if any, supports most of them.
Palmitoylethanolamide (PEA)
Palmitoylethanolamide (PEA) is a
N-acylethanolamine molecule in a family of long-chain fatty acid
 amides
called ALIAmides. PEA has been found in rat and mice studies to limit
hyperactvity in immune cells and thereby control inflammatory responses
and resulting tissue damage. PEA is produced by the animal's body as
needed in response to certain types of injuries. PEA is a product of
normal fatty acid synthesis from palmitic acid. It is found in many
common foods, particularly palm oil, soy beans, egg yolks, and peanuts.
The commercial version is most commonly manufactured from palm oil*.
amides
called ALIAmides. PEA has been found in rat and mice studies to limit
hyperactvity in immune cells and thereby control inflammatory responses
and resulting tissue damage. PEA is produced by the animal's body as
needed in response to certain types of injuries. PEA is a product of
normal fatty acid synthesis from palmitic acid. It is found in many
common foods, particularly palm oil, soy beans, egg yolks, and peanuts.
The commercial version is most commonly manufactured from palm oil*.
Not all PEA is alike. There are at least 4 types of PEA, and the differences of those 4 are described below here. The differences are mainly the sizes of the particles. The larger the size of particle, the less soluble and less bioavailable. Micronization reduces the size of the particles of PEA. In short, since the basic (naïve) PEA is almost totally insoluble in water and therefore has very poor bioavailability, researchers use micronized or ultra-micronized PEA or water-dispersible PEA in their published studies.
• Basic PEA, called "naïve PEA", is almost totally insoluble in water and under gastrointestinal conditions and therefore the oral intake of it (rather than being injected directly into the abdomen) has very poor bioavailability, meaning that it does not get absorbed well in the dog's gut. See this May 2021 article and this July 2025 article.
• Micronized PEA (m-PEA or micro-palmitoylethanolamide) is a patented technique that reduces the diameter of PEA particles, making them absorbable in the intestine, which has been found to be more effective than ordinary basic PEA in activating PEA levels in blood plasma in dogs. See this August 2014 article.
• Ultra-micronized PEA (um-PEA), also patented, reduces the PEA particle size further, to enable it to cross the blood-brain barrier, likewise has been found to be much more effective than basic PEA. See this August 2014 article.
• Water-Dispersible PEA (PEA-WD), also patented, reduces the PEA to a powder which can be dispersed in cold water. It has been found to be 16 times more effective than basic PEA. See this July 2025 article.
• Hybrid versions of PEA: Additionally, PEA has been combined with other ingredients and used in some published studies. These include FenuMat-PEA (P-fen), which is a PEA hybrid combined with the herb fenugreek (trigonella foenum-graecum), and hybrids combined with resveratrol, quercetin, fisstin, and boswellic acid. See this May 2025 article and this July 2025 article.
 If a PEA product is not advertised as being micronized or
ultra-micronized, then
Dr. Clare Rusbridge advises that
"You
probably are wasting your money."
A variety of brands of
micronized and ultra-micronized PEA are offered on-line.
If a PEA product is not advertised as being micronized or
ultra-micronized, then
Dr. Clare Rusbridge advises that
"You
probably are wasting your money."
A variety of brands of
micronized and ultra-micronized PEA are offered on-line.
Dogs affected by atopic dermatitis (AD) have been found to have significantly elevated levels of their self-produced PEA, when compared to dogs without AD. This indicates the "on demand" aspect of PEA, that the dog produces more of its own PEA when needed to combat inflammation and other causes of skin eruptions. See this January 2014 article.
In an August 2015 article sponsored by the major supplier of PEA (Innovet Italia), Italian researchers conducted an 8-week study of the effectiveness of oral ultra-micronized palmitoylethanolamide (um-PEA) in 160 dogs with moderate atopic dermatitis. Each dog received a daily dose of um-PEA at the rate of 10 mg/kg for 56 days. The investigators concede some major limitations in the study but conclude that the number of participating dogs -- 160 -- offsets those limitations. They concluded:
"Notwithstanding the above limitations, our findings suggest that PEA-um, within a multifaceted and integrated therapeutic approach for cAD [canine atopic dermatitis], may be a promising treatment for dogs with moderate atopic dermatitis and moderate pruritus, with consequent improvement in QoL [quality of life]."
By "multifaceted and integrated therapeutic approach", they meant that the um-PEA was given in combination with more conventional AD medications.
Read more about PEA on our PEA webpage.
* Palm oil: The palm oil cultivation industry has been destroying rainforests in Sumatra and Borneo in Indonesia and Malaysia, the only habitats of orangutans. If you are going to obtain PEA, we suggest that you do so only from vendors whose PEA has been manufactured with palm oil from sustainable sources and not the deforestation of rainforests. TRead more about finidng sources of sustainable palm oil at www.orangutanlandtrust.com. To avoid palm oil as the source of PEA, read the ingredients descriptions on the brands of PEA in which you are interested.
RETURN TO TOP
Cannabinol (CBD oil)
 Cannabinol (CBD
oil) is produced from hemp and marijuana (Cannabis
Sativa) plants. CBD oil mimics the endocannabinoid molecules which the
dog’s (and our) body produces in several different organs. They play
roles in reducing pain, regulating inflammation, and affecting the
immune system, by initially binding to receptors in the brain.
Recommended dosages very widely, from 0.25 mg per kg per day to as much
as 9 mg/kg/day (for epilepsy). However, the maximum recommended dose for
adult humans is only 0.15 mg/kg/daily, the equivalent of 5 drops of 5%
CBD oil.
Cannabinol (CBD
oil) is produced from hemp and marijuana (Cannabis
Sativa) plants. CBD oil mimics the endocannabinoid molecules which the
dog’s (and our) body produces in several different organs. They play
roles in reducing pain, regulating inflammation, and affecting the
immune system, by initially binding to receptors in the brain.
Recommended dosages very widely, from 0.25 mg per kg per day to as much
as 9 mg/kg/day (for epilepsy). However, the maximum recommended dose for
adult humans is only 0.15 mg/kg/daily, the equivalent of 5 drops of 5%
CBD oil.
Varieties of CBD: Cannabidiol-based veterinary products are derived mainly from hemp (Cannabis sativa) and must contain less than 0.3% tetrahydrocannabinol (THC). This form of CBD can be processed into “full spectrum” or “broad spectrum” and also may be in the form of a “distillate”, in which all THC has been removed, or in the form of CBD “isolate”, which is a purifed powder.
• Full Spectrum: Full spectrum CBD contains other extracts found in the cannabis plant, including terpenes, and up to 0.3% THC.
• Broad Spectrum: Broad spectrum CBD also contains some other cannabis compounds but no more than trace amounts of THC.
• CBD Isolate: CBD isolate is pure CBD and contains no other cannabis plant compounds.
• Naked CBD: Naked CBD describes CBD oil by itself, as opposed to being capsultated or microcapsulated or combined with any other substance, such as deoxycholic acid (DCA).
• Liposomal CBD: This is an orally administered encapsultated CBD which is packaged within liposomes, small fatty cellular sacs which improve bioavailability of the CBD by enabling it to be withstand digesstion in the stomach and degradation in the liver. Lipsomal CBD was tested on dogs in this September 2020 article.
• Cannabidiolic acid (CBDA) is an acid precursor of CBD. It forms CBD when heated. It has been shown in some studies to be more potent that CBD for treating rats. It has been found to be more readily absorbed into the human bloodstream than CBD. Aa theory is that adding CBDA to doses of CBD may make the CBD more absorbable. In this September 2020 article, the investigators found that CBDA is absorbed at least twice as well as CBD in dogs within a 24 hour period, with some differences depending upon the medium used to deliver the oral treatment.
 Thus far, the results of published studies in which cannabinoids
(CBD) have been used to treat this skin disorder have been mixed.
Thus far, the results of published studies in which cannabinoids
(CBD) have been used to treat this skin disorder have been mixed.
CBD and cannabidiolic acid (CBDA) were involved in a 2021 pilot study invoving 17 dogs diagnosed with atopic dermatitis. None were cavaliers. All continued to be treated also with conventional medications. The dogs were given an oral dose of CBD-rich and CBDA-rich hemp in sesame oil for four weeks. Subjective measurements of inflammation using the Canine Atopic Dermatitis Scoring Index and owners subjective scaling asseessments of pruritus were performed.
The dogs were administered CBD/CBDA (approximately 2 mg/kg) twice a day with a meal for the 28-day study period. The investigators report that a bare majority of the 17 dogs in the treatment group showed measurable decreases in pruritus. They listed these symptoms as "adverse events": lethargy, increased flatulence, inconsistent appetite, somnolence, sleepiness, decreased aggression, increased calmness, and increased energy/mobility.
During the 4 weeks, since the dogs also were treated with conventional medications, the investigators concluded by suggesting tht CBD be an "adjunct therapy". They stated:
"Our results suggest that CBD as an adjunct therapy is useful in decreasing pruritus in some dogs with cAD [canine atopic dermatitis]. CBD at 2 mg/kg twice daily was well-tolerated with minimal AEs [adverse events].
An April 2022 article reports the results of testing CBD on 8 dogs suffering from canine atopic dermatitis (CAD) over a period of 8 weeks. The investigators noted clinical improvement in both CADESI-4 and pruritus scores in the dogs treated with THC-free CBD oil twice daily for 8 weeks. The dogs also continued to be treated with other medications (including oclacitinib, anixucukkub, prednisolone, and ketoconazole).
To the contrary, in an October 2023 article, 7 dogs diagnosed with canine atopic dermatitis (CAD) were treated only with full spectrum high cannabidiol (CBD) cannabis oil, 2.5 mg/kg for 6 weeks. They report finding: "This study reveals that the full-spectrum cannabis oil rich in CBD at a dosage of 2.5 mg/kg does not show therapeutic advantage when compared to olive oil. "
See our Cannabis webpage for additional details about CBD, including delivery methods, bioavailability, dosages, and adverse reactions.
Vitamin D
Vitamin D supplementation reportedly may aid in relief of CAD.
RETURN TO TOP
Fecal Microbiota Transplantation (FMT)
 Fecal Microbiota Transplantation (FMT) is a process of stool
transplanting, whereby fecal material from a healthy donor dog is
inserted into the anus of the patient, a medical procedure called
endoscopy or rectal enema, or is given orally using a syringe or in a capsule.
The fecal material is either fresh or freeze-dried. The
purpose of this procedure is to supplement or replace the gut microbiota
in the dog's intestines, to increase the number and varieties of
beneficial bacteria to restore the proper function of the gut
microbiota.
Fecal Microbiota Transplantation (FMT) is a process of stool
transplanting, whereby fecal material from a healthy donor dog is
inserted into the anus of the patient, a medical procedure called
endoscopy or rectal enema, or is given orally using a syringe or in a capsule.
The fecal material is either fresh or freeze-dried. The
purpose of this procedure is to supplement or replace the gut microbiota
in the dog's intestines, to increase the number and varieties of
beneficial bacteria to restore the proper function of the gut
microbiota.
FMT is being studied as a treatment for canine atopic dermatitis. In a May 2023 article, a single fresh dose of fecal material was delivered orally by syringe to 12 dogs, including a cavalier, all of which had been diagnosed with canine atopic dermatitis (cAD). Thje dogs then were examined on day 28 and day 56. The investigators reported:
"In conclusion, the present study revealed that a single oral FMT significantly decreased skin lesions and pruritus scores and changed the gut microbiota in dogs with AD. Since this study was designed as a pilot trial with a short observation period (56 days), further studies are needed to clarify the long-term effect of a single or repeated oral FMT on cAD using a large population of dogs with mild to severe AD and appropriate controls. Nevertheless, this study provides evidence for a crucial role of the gut microbiota in the pathogenesis and a therapeutic target of cAD."
As for the effectiveness of FMT treatments using oral capsules, in a January 2024 article, in which 54 dogs were studied, fresh fecal material was orally given by capsule for 25 days. On average, only 18% of the stool donor’s bacterial amplicon sequence variants (ASVs) engrafted in the FMT recipient.
RETURN TO TOP
Veterinary Specialists
The American College of Veterinary Dermatology (ACVD) certifies
dermatology specialists. Find a veterinary
 dermatologist
on
the ACVD website at this link.
dermatologist
on
the ACVD website at this link.
The ACVD is empowered to examine qualified candidates and confer Diplomate (board certification) status in veterinary dermatology. Board certification requires completion of a 2-3 year approved residency training program, an original research project, publication in a scientific journal, and successful completion of the certification examination. Currently there are about three hundred ACVD board certified veterinary dermatologists worldwide who work in private specialty practices, academic positions, and industry.
RETURN TO TOP
Research News
October 2024:
Cavalier is diagnosed with alopecia areata and
uveodermatological syndrome.
 In
an
October 2024 article, a team of American clinicans (Barbara G.
McMahill [right], Sophie Gilbert, Jamie Haddad, Janelle Novak,
Maria Shank, and Verena K. Affolter) report a case study of a year old
female cavalier King Charles spaniel they diagnosed with both alopecia
areata and
uveodermatological syndrome. Alopecia
areata (AA) is an immune system disfunction which attacks the dog's hair
follicles, causing hair loss, usually in patches. “Alopecia” is the
medical term for hair loss, and “areata” means that it occurs in small,
random areas. In dogs, it may be associated with diabetes or thyroid
disease. AA is not curable, but medications and other treatments help
manage the hair loss, and while treated, hair may regrow. Treatments
usually include corticosteroids, immunotherapies, and phototherapy. They describe the dog's
signs, diagnosis, treatment, and clinical follow-up. See our
Eyes webpage for a
discussion of uveodermatological syndrome.
In
an
October 2024 article, a team of American clinicans (Barbara G.
McMahill [right], Sophie Gilbert, Jamie Haddad, Janelle Novak,
Maria Shank, and Verena K. Affolter) report a case study of a year old
female cavalier King Charles spaniel they diagnosed with both alopecia
areata and
uveodermatological syndrome. Alopecia
areata (AA) is an immune system disfunction which attacks the dog's hair
follicles, causing hair loss, usually in patches. “Alopecia” is the
medical term for hair loss, and “areata” means that it occurs in small,
random areas. In dogs, it may be associated with diabetes or thyroid
disease. AA is not curable, but medications and other treatments help
manage the hair loss, and while treated, hair may regrow. Treatments
usually include corticosteroids, immunotherapies, and phototherapy. They describe the dog's
signs, diagnosis, treatment, and clinical follow-up. See our
Eyes webpage for a
discussion of uveodermatological syndrome.
August 2024: Long-term heavy doses of cyclosporine treatment cause severe dermatosis in a cavalier. In an August 2024 article, a team of Japanese clinicians (Junko Ike, Ryosuke Ueda, Takeshi Mukosaka, Maiko Sekiguchi, Toshiroh Iwasaki) reported case studies of 4 dogs diagnosed with psoriasiform-lichenoid dermatosis associated with treatment for several months with cyclosporine for immune-mediated diseases. One of these dogs was a 7 year old cavalier being given oral cyclosporine and pednisolone (for polyarthritis) for 7 months. The cavalier developed chronic eczema with lichenoid plaques, scales, and hyperpigmentation, and hair loss around its eyes, mouth, and abdomen after 5 months of treatment. At that point, the prednisolone was discontinued, but the dermatitis continued. The clinicians treated the cavalier with amoxicillin, a penicillin antibiotic used to treat bacterial infections for a week, and bathed with a salicylic acid shampoo and moisturizer, all with no improvement. They then reduced the dosage of cyclosporine by half (from 17.5 to 8.8 mg/kg/day). Three weeks later, hair began to grow again around the mouth and body. After 8 weeks, the lichenoid plaques, scales and hyperpigmentation had almost disappeared. The dog died 3.5 months later due to an unspecified unrelated cause. He was diagnosed with psoriasiform-lichenoid dermatosis accompanied by cocci proliferation and infection, induced by cyclosporine. The clinicians concluded that psoriasiform-lichenoid dermatosis may develop in dogs receiving high dosage or long-term administration of cyclosporine.
RETURN TO TOP
Related Links
RETURN TO TOP
Veterinary Resources
Alopecia areata:
Uveodermatological syndrome associated with alopecia areata in a
one-year-old female spayed Cavalier King Charles Spaniel
dog.
 Barbara G. McMahill, Sophie Gilbert, Jamie Haddad,
Janelle Novak, Maria Shank, Verena K. Affolter. Vet. Derm. October
2024; doi: 10.1111/vde.13303. Quote: Uveodermatological syndrome and
alopecia areata are autoimmune disorders causing ocular and
dermatological inflammation and alopecia, respectively, in dogs.
This is the first report to document concurrent development of the
two diseases in a dog, as has been reported in human patients.
Clinical presentation and histopathological diagnosis, treatment and
clinical follow-up are described. ... A 1. 5-year-old female spayed
tri-colour Cavalier King Charles Spaniel was presented with a
five-months history of progressive alopecia and depigmentation.
Eight months previously, the dog had been diagnosed with bilateral
uveitis and keratoconjunctivitis sicca, resulting in bilateral
glaucoma. At that time, partial depigmentation of the nasal planum
and periocular skin were the only cutaneous signs noted. ... Upon
presentation to the dermatologist, multifocal areas of progressive
alopecia on the thorax, flanks, abdomen and at the tail base were
noted. ... Figure (a) Distribution of alopecia, poliosis and
leukoderma along base of tail, flanks, thorax and abdomen. Note only
black‐haired areas are affected.
Barbara G. McMahill, Sophie Gilbert, Jamie Haddad,
Janelle Novak, Maria Shank, Verena K. Affolter. Vet. Derm. October
2024; doi: 10.1111/vde.13303. Quote: Uveodermatological syndrome and
alopecia areata are autoimmune disorders causing ocular and
dermatological inflammation and alopecia, respectively, in dogs.
This is the first report to document concurrent development of the
two diseases in a dog, as has been reported in human patients.
Clinical presentation and histopathological diagnosis, treatment and
clinical follow-up are described. ... A 1. 5-year-old female spayed
tri-colour Cavalier King Charles Spaniel was presented with a
five-months history of progressive alopecia and depigmentation.
Eight months previously, the dog had been diagnosed with bilateral
uveitis and keratoconjunctivitis sicca, resulting in bilateral
glaucoma. At that time, partial depigmentation of the nasal planum
and periocular skin were the only cutaneous signs noted. ... Upon
presentation to the dermatologist, multifocal areas of progressive
alopecia on the thorax, flanks, abdomen and at the tail base were
noted. ... Figure (a) Distribution of alopecia, poliosis and
leukoderma along base of tail, flanks, thorax and abdomen. Note only
black‐haired areas are affected.
Black hair follicular dysplasia:
Black hair follicular dysplasia [in dogs]. K. A. Dunn, M. Russell, J. M. Boness. Vet. Rec. December 1995; 137(16):412. Quote: Cases of the condition in a largely black, male, 10-year-old border Collie and a 3-year-old tricoloured, female Cavalier King Charles Spaniel are reported. The Collie had a history of chronic skin problems including pruritus responsive to prednisolone in dark haired areas only, the spaniel had a poor fluffy haircoat affecting only dark haired areas. Biopsies of affected areas showed characteristic changes. This is apparently the first report of the condition in a Cavalier King Charles Spaniel and only the third report in a Border Collie.
Canine atopic dermatitis:
Breed and site predispositions of dogs with atopic dermatitis: a comparison of five locations in three continents. K. Jaeger, M. Linek, H.T. Power, S.V. Bettenay, S. Zabel, R.A.W. Rosychuk, Ralf S. Mueller. Vet. Dermatology. February 2010;21(1):119-123. Quote: "The objectives of this multicentre study were to analyse and compare breed predispositions and lesion distributions of 552 dogs diagnosed with atopic dermatitis from five different dermatologic referral centres located in Australia, Germany (2) and the United States (2). Breeds were compared with the canine population in the respective locations. Breed predispositions varied from geographical site, although golden retrievers and German shepherd dogs were predisposed in three of five practices. [Cavalier King Charles spaniels were predisposed in Australia.] Lesions were present most commonly on the paws (62%), ventrum (51%), ears (48%) and face (39%). Various breeds had specific site predilections. Based on this study, breed predispositions can vary greatly both between continents and also between different locations on the same continent. In addition, some breeds showed predispositions for certain body sites which also varied in some instances with the geographical location.
Treatment of canine atopic dermatitis: 2010 clinical practice guidelines from the International Task Force on Canine Atopic Dermatitis. Thierry Olivry, Douglas J. DeBoer, Claude Favrot, Hilary A. Jackson, Ralf S. Mueller, Tim Nuttall, Pascal Prélaud. Vet. Derm. May 2010; doi: 10.1111/j.1365-3164.2010.00889.x. Quote: Atopic dermatitis (AD) is a common chronic relapsing pruritic skin disease of dogs for which treatment has varied over time and geographical location. Recent high quality randomized controlled trials and systematic reviews have established which drugs are likely to offer consistent benefit. The International Task Force for Canine AD currently recommends a multi-faceted approach to treat dogs with AD. Acute flares should be treated with a combination of nonirritating baths and topical glucocorticoids, once an attempt has been made to identify and remove the suspected causes of the flare. Oral glucocorticoids and antimicrobial therapy must be added when needed. In dogs with chronic AD, a combination of interventions should be considered. Again, factors that trigger flares of AD must be identified and, if possible, avoided. Currently recognized flare factors include food, flea and environmental allergens, Staphylococcus bacteria and Malassezia yeast. Skin and coat hygiene and care must be improved by bathing with nonirritating shampoos and dietary supplementation with essential fatty acids. The severity of pruritus and skin lesions can be reduced with a combination of anti-inflammatory drugs. Currently, medications with good evidence of high efficacy include topical and oral glucocorticoids, and calcineurin inhibitors such as oral ciclosporin and topical tacrolimus. The dose and frequency of administration of these drugs should be tailored to each patient considering each drug’s efficacy, adverse effects and cost. Allergen-specific immunotherapy should be offered, whenever feasible, in an attempt to prevent recurrence of clinical signs upon further exposure to environmental allergens to which the patient is hypersensitive.
Micronized/ultramicronized palmitoylethanolamide displays superior oral efficacy compared to nonmicronized palmitoylethanolamide in a rat model of inflammatory pain. Daniela Impellizzeri, Giuseppe Bruschetta, Marika Cordaro, Rosalia Crupi, Rosalba Siracusa, Emanuela Esposito, Salvatore Cuzzocrea. Neuroinflammation. August 2014; doi: 10.1186/s12974-014-0136-0. Quote: Background: The fatty acid amide palmitoylethanolamide (PEA) has been studied extensively for its anti-inflammatory and neuroprotective actions. The lipidic nature and large particle size of PEA in the native state may limit its solubility and bioavailability when given orally, however. Micronized formulations of a drug enhance its rate of dissolution and reduce variability of absorption when orally administered. The present study was thus designed to evaluate the oral anti-inflammatory efficacy of micronized/ultramicronized versus nonmicronized PEA formulations. Methods: Micronized/ultramicronized PEA was produced by the air-jet milling technique, and the various PEA preparations were subjected to physicochemical characterization to determine particle size distribution and purity. Each PEA formulation was then assessed for its anti-inflammatory effects when given orally in the carrageenan-induced rat paw model of inflammation, a well-established paradigm of edema formation and thermal hyperalgesia. Results: Intraplantar injection of carrageenan into the right hind paw led to a marked accumulation of infiltrating inflammatory cells and increased myeloperoxidase activity. Both parameters were significantly decreased by orally given micronized PEA (PEA-m; 10 mg/kg) or ultramicronized PEA (PEA-um; 10 mg/kg), but not nonmicronized PeaPure (10 mg/kg). Further, carrageenan-induced paw edema and thermal hyperalgesia were markedly and significantly reduced by oral treatment with micronized PEA-m and ultramicronized PEA-um at each time point compared to nonmicronized PeaPure. However, when given by the intraperitoneal route, all PEA formulations proved effective. Conclusions: These findings illustrate the superior anti-inflammatory action exerted by orally administered, micronized PEA-m and ultramicronized PEA-um, versus that of nonmicronized PeaPure, in the rat paw carrageenan model of inflammatory pain.
Review: Clinical and histological manifestations of canine atopic dermatitis. Petra Bizikova, Domenico Santoro, Rosanna Marsella, Tim Nuttall, Melissa N. C. Eisenschenk, Cherie M. Pucheu-Haston. Vet. Dermatology. February 2015. Quote: "Background: Many studies focusing on clinical and histological signs of canine atopic dermatitis (AD) have been published since its early descriptions decades ago. Findings of these studies contributed to our current knowledge about the disease pathogenesis and allowed establishment of diagnostic criteria used by clinicians and researchers. Objectives: This review serves as an update on the clinical and histological features of canine AD published by the American College of Veterinary Dermatology Task Force on Canine Atopic Dermatitis in 2001 and summarizes the recent discoveries in these fields. Results: The overall findings of studies focusing on clinical features mirrored those published by the Task Force in 2001. The novelty was the larger number of animals included in these studies, which allowed establishment of a new set of diagnostic criteria that exceeded the sensitivity and specificity of the previous criteria. The same study uncovered some clinical differences between dogs with food-induced and nonfood-induced AD; however, the authors concluded that these two entities cannot be distinguished based on clinical signs only. Another study demonstrated some major breed-specific phenotypes. Several publications addressed the histological features of canine AD skin lesions in experimental models of AD, but none of those addressed naturally occurring lesions. Nevertheless, the histopathological description of the skin reactions was generally similar to that published by the Task Force in 2001. Conclusions: Considerable work has been done in recent years to provide a better definition of the clinical appearance and histopathology of canine AD. New sets of diagnostic criteria have been developed, and additional breed-associated differences in phenotypes have been demonstrated.
Increased numbers of peripheral blood CD34+ cells in dogs with canine atopic dermatitis. Vincent Bruet, Blandine Lieubeau, Julie Herve, Anne Roussel, Laëtitia Imparato, Jean-Claude Desfontis, Patrick Bourdeau. Vet. Dermatology. June 2015;26(3):160-e33. Quote: "Background: The bone marrow may be involved in human atopic diseases, as shown by the release of CD34+ cells into the peripheral blood. Hypothesis/Objectives: The aim was to determine the numbers of CD34+ cells in atopic dogs. Animals: The following three groups of dogs were studied: 27 dogs with nonfood-induced atopic dermatitis (NFICAD)[including a cavalier King Charles spaniel]; 16 dogs with nonallergic inflammatory diseases; and 13 healthy control dogs [including a cavalier King Charles spaniel]. Methods: Dogs with NFICAD were selected after fulfilment of Favrot's criteria and exclusion of other pruritic dermatoses, including flea infestation and adverse reaction to foods. The Canine Atopic Dermatitis Extent and Severity Index (CADESI)-03 and a Visual Analog Scale (VAS) score for pruritus were used to quantify clinical signs. A phycoerythrin-conjugated anticanine CD34 antibody was used to stain peripheral blood CD34+ cells, and these were enumerated using a flow cytometer. The CD34+ cell counts were compared between groups and tested (in the NFICAD group) for correlation with the severity of clinical signs. Results: The numbers of peripheral CD34+ cells in dogs with NFICAD (median 1.7) were statistically higher than in dogs with other nonallergic inflammatory diseases (median 1.0; P = 0.01) and healthy control dogs (median 0.9; P = 0.009). In dogs with NFICAD, there was no correlation between CD34+ cell numbers and CADESI-03 scores or owner-assessed pruritus (VAS score). Conclusions and clinical importance: The results of this study suggest the possible involvement of CD34+ cells in dogs with NFICAD. The role of CD34+ cells in the aetiopathogenesis of canine atopic dermatitis remains to be determined."
Long-term compassionate use of oclacitinib in dogs with atopic and allergic skin disease: safety, efficacy and quality of life. Sallie B. Cosgrove, Dawn M. Cleaver, Vickie L. King, Amy R. Gilmer, Anne E. Daniels, Jody A. Wren, Michael R. Stegemann. Vet. Dermatology. June 2015;26(3):171-e35. Quote: Background: Oclacitinib is safe and effective for treating dogs with pruritus associated with allergic and atopic dermatitis, based on randomized clinical trials of up to 4 months duration. Hypothesis/Objectives: This study assessed long-term safety, efficacy and quality of life of oclacitinib-treated dogs enrolled in a compassionate use programme. Animals: Two hundred and forty-seven client-owned dogs with allergic skin disease that had previously benefited from oclacitinib therapy [including cavalier King Charles spaniels]. Methods: Dogs were enrolled in an open-label study at 26 veterinary clinics. Dogs received 0.4–0.6 mg/kg oclacitinib twice a day for 14 days, then once a day for up to 630 days. Assessments were performed at ~90 day intervals. Owners completed a quality-of-life survey and assessed pruritus using a Visual Analog Scale (VAS) at each clinic visit. Veterinarians assessed dermatitis using a similar VAS. Abnormal health events, concomitant medication and clinical pathology results were summarized. Results: Visual Analog Scale scores showed improvement from baseline at all time points. The percentage of dogs showing ≥50% reduction from baseline on day 90 was 63.9% for pruritus and 66.4% for dermatitis. Owners saw a positive impact on quality of life in >91% of all dogs. Urinary tract infection/cystitis, vomiting, otitis, pyoderma and diarrhoea were the most frequently reported (>5% of dogs) abnormal clinical signs. Haematology and serum chemistry means remained within the normal reference ranges. Concomitant medications were well tolerated. Conclusions and clinical importance: Results indicated that oclacitinib was safe and efficacious for long-term use and improved the quality of life for dogs in this study.
Efficacy of ultra-micronized palmitoylethanolamide in canine atopic
dermatitis: an open-label multi-centre study. Chiara Noli,
M. Federica della Valle, Alda Miolo, Cristina Medori, Carlo
Schievano. Vet. Dermatol. August 2015; doi: 10.1111/vde.12250.
Quote: Background: Palmitoylethanolamide is a naturally occurring
bioactive lipid, produced on-demand by damage-exposed cells.
Palmitoylethanolamide is documented to counteract inflammation, itch
and pain. Objective: The aim of this 8-week study was to evaluate
the efficacy of oral ultra-micronized palmitoylethanolamide (PEA-um)
in dogs with moderate atopic dermatitis. Animals: Clinicians from 39
veterinary clinics enrolled 160 dogs with nonseasonal atopic
dermatitis and moderate pruritus. Methods: This was a multi-centre
open-label study. On days 0 (D0) and 56 (D56), owners evaluated
pruritus with a Visual Analog Scale (VAS) and completed a validated
Quality of Life (QoL) questionnaire. Veterinarians assessed the
severity of skin lesions using the Canine Atopic Dermatitis Lesion
Index (CADLI). Results: Mean pruritus VAS score decreased from 5.7 ±
0.08 cm (range 3.8–7.9 cm) to 3.63 ± 0.19 cm (range 0.1–9.2 cm) (P <
0.0001). At D56, 58% of dogs showed a greater than 2 cm reduction
from baseline and 30% showed an absent-to-very mild pruritus (VAS ≤
2 cm). Mean total CADLI at D56 decreased significantly (P < 0.0001);
in 62% of dogs this score reached a value in the remission range
(≤5). Mean total QoL score was significantly decreased (P < 0.0001)
with 45% of dogs reaching QoL values described for healthy animals.
Tolerability was good-to-excellent with only four dogs reporting
treatment associated reversible adverse events. Conclusions and
clinical importance:
PEA-um appears to be effective and safe in
reducing pruritus and skin lesions, and in improving QoL in dogs
with moderate atopic dermatitis and moderate pruritus.
Lokivetmab improved pruritus in a dog with cutaneous epitheliotropic lymphoma. Kiyohiko Inai, Keita Kitagawa, Mami Murakami, Toshiroh Iwasaki. J. Vet. Med. Sci. January 2022; doi: 10.1292/jvms.21-0346. Quote: A 13-year-old spayed female Cavalier King Charles Spaniel presented with chronic swelling and pruritus on the palmar aspect of the left forepaw and on the tail. Cutaneous epitheliotropic lymphoma (CEL) was diagnosed by histopathology and immunocytochemistry. Prednisolone was initially used alone as an alternative treatment for CEL. Despite long-term corticosteroid therapy, the patient’s physiological (pruritus) and dermatological signs (alopecia, erythema, erosion, and ulceration with crust) progressed and showed no evidence of improvement. ... In the hope of mitigating this ongoing pruritus, lokivetmab (1.25 mg/kg, SC, once) was initiated in combination with prednisolone (1.5 mg/kg, PO, q24 hr). On Day 112, facial alopecia with crusting was still present. The ulcerative lesions remained unchanged with no remarkable improvement. Despite the patient’s minimal clinical response, the [pruritus visual analogue scale] (PVAS) score was found to be 7. A decision was made to further taper the dose of prednisolone to 1 mg/kg, PO, q24 hr. The PVAS score fell from 5 to 3 in two weeks. On Day 132, one month after starting lokivetmab, the pruritus subsided. To prevent the possibility of relapse, lokivetmab (1.25 mg/kg, SC, once) was re-administered. On Day 153, despite the persistence of the facial alopecia with crusting, the PVAS score had dropped to 2, suggesting the pruritus was now well-controlled. On Day 160, the pruritus was controlled with a PVAS score of 1. Since the pruritus was negligible, active monitoring was initiated without further treatment of lokivetmab. Hair started to regrow on the face where alopecia was previously reported. On Day 167, the pruritus remained stable with a PVAS score of 1. Since the last visit, the patient sustained an excellent quality of life and eventually passed away due to progressive lymphoma on Day 183.
 (A)
(A) On Day 14, nasal depigmentation had emerged. (B) On Day 105,
progression of facial alopecia with crusting was found. (C) On Day
132, facial alopecia with crusting was still present. (D) On Day
160, hair regrew on the face where alopecia was present.
(A)
(A) On Day 14, nasal depigmentation had emerged. (B) On Day 105,
progression of facial alopecia with crusting was found. (C) On Day
132, facial alopecia with crusting was still present. (D) On Day
160, hair regrew on the face where alopecia was present.
In this dog, there was no history of CAD or cutaneous adverse food reactions before the age of 8, and the patient’s pruritus worsened as skin lesions progressed over time despite the use of prednisolone. Therefore, in this case the pruritus was considered to be related to CEL. IL-31 is produced mainly by activated T cells, and it is a critical pruritogenic cytokine associated with atopic dermatitis in humans and dogs. It has been reported that the serum concentrations of IL-31 were not statistically different between non-pruritic dogs with CEL and healthy controls. However, the contribution of IL-31 to pruritus in dogs with cutaneous lymphoma has not been fully understood in veterinary medicine. ... Lokivetmab, a monoclonal antibody used to treat CAD, is reported to neutralize IL-31 and mitigate canine pruritus. Although lokivetmab is not indicated for the treatment of CEL, it was used in the hope of reducing pruritus. In this case of CEL, lokivetmab decreased pruritus. Thus, anti-IL-31 therapy appears to be a potential treatment option in controlling pruritus associated with CEL in dogs. ... Further investigation on the critical role of IL-31 in the pruritus pathway of dogs with CEL is required.
Antibacterial activity of cannabis extract (Cannabis sativa L. subsp. indica (Lam.)) against canine skin infection bacterium Staphylococcus pseudintermedius. Jareerat Aiemsaarda, Ranee Singh, Glenn N. Borlace, Bungorn Sripanidkulchai, Peera Tabboon, Eakachai Thongkham. Sci. Asia, February 2022; doi: 10.2306/scienceasia1513-1874.2022.053. Quote: Superficial bacterial skin infections caused by Staphylococcus pseudintermedius are common in dogs. The cannabis plant has shown potential antibacterial effects, but there is limited information about anti-S. pseudintermedius activity. This study investigated the antibacterial activity of the ethanolic extract and the topical formulations of Cannabis sativa L. subsp. indica (Lam.) against 23 S. pseudintermedius isolates obtained from canine pyoderma using broth microdilution and time-kill assays. The cannabis extract’s minimum inhibitory concentrations for 50% (MIC50) and 90% (MIC90) of the tested S. pseudintermedius isolates were 6.25 and 12.50 µg/ml, respectively. The MIC for S. pseudintermedius ATCC 49051 was 6.25 µg/ml. The time-kill test revealed that the bactericidal effect of the cannabis extract was time- and not concentration-dependent. Topical formulations containing 0.5, 1, 2, 5, and 10% w/w cannabis extract showed limited in vitro antimicrobial activity in the time-kill test. Only the formulations with cannabis extract of 10% and 5% w/w could reduce the number of viable S. pseudintermedius ATCC 49051 by more than 3-log10 (99.9%) at 6 and 24 h, respectively. This study demonstrated that the cannabis extract has a good potential to be developed as an antibacterial agent against S. pseudintermedius. However, a clinical trial should be conducted to determine its in vivo therapeutic efficacy.
Effects of cannabidiol without delta-9-tetrahydrocannabinol on canine atopic dermatitis: a retrospective assessment of 8 cases. Chie Mogi, Masanori Yoshida, Koji Kawano, Takaaki Fukuyama, Toshiro Arai. Can. Vet. J. April 2022;63(4):423-426. Quote: Objective: We aimed to examine the effects of cannabidiol (CBD)-containing hemp oil without delta-9-tetrahydrocannabinol (THC) as a supplemental treatment for canine atopic dermatitis (CAD), as well as its adverse effects, and effects on concurrent drug use in dogs. Animal: In this retrospective case series, 8 dogs with CAD [none being cavaliers] were diagnosed by veterinary dermatologists certified by the Japanese Society of Veterinary Dermatology. Procedure: The medical records of dogs supplemented with CBD-containing hemp oil were evaluated with respect to signalment, physical examination, plasma C-reactive protein concentrations, pharmacologic management, the CAD Extent and Severity Index (4th iteration), and the Pruritus Visual Analog Scale. ... We administered a 10% CBD-containing broad-spectrum hemp oil (Mary’s Tails Hemp Extract Tincture; Mary’s Nutritionals, Denver, Colorado, USA) to the 8 dogs with CAD for at least 8 wk. Each dog received oral administrations q12h for the entire study period at a dose of 0.14 to 1.43 mg/kg/d. These CBD products were certified to not contain THC. ... According to the CBD manufacturer’s information, all dogs were started at a dose of approximately 0.07 to 0.25 mg/kg of body weight twice daily. During the testing period, the dose was increased depending on the skin condition of each dog and the observed response at 0.125 mg/kg. The dose was increased if no apparent change was observed with the previous dose. Concomitant medications were allowed during the study period, and their doses could be maintained or reduced by the certified dermatologist on Day 0. ... No adverse events were reported following ingestion of the CBD oil. Improvements were noticed in each dog, as described in the following paragraphs. Due to the absence of a control group, we could not conclude whether the improvements were caused fully or in part by the CBD. The CADESI values decreased in 5 dogs, remained unchanged in 1 dog, and increased in 1 dog. The PVAS values decreased in 7 dogs but increased in 1 dog. ... In the present study, improvements in pruritic behavior were observed in all dogs, which may have been related to the use of CBD. However, the lack of a control group is one of the main limitations of this study, which restricted the conclusions regarding the efficacy of CBD. ... Results: Overall, CBD, used as a supplement in combination with other drugs, was well-tolerated over a wide dose range and decreased the occurrence of pruritus in dogs with CAD when ingested twice a day. ... Although the number of cases was limited, we tested a new treatment method with the aim of examining the safety of combining a CBD supplement with therapeutic drugs, with a lack of adverse events following administration of CBD. Furthermore, there was a decrease in the frequency of concomitant medication use and an improvement in quality of life and symptoms, suggesting that a new approach using supplementary CBD could improve the quality of life for dogs as well as their owners. ... Conclusion: This study provides the first report of supplementation with CBD without THC that was effective in controlling pruritic behavior in dogs with CAD. Clinical relevance: Further controlled studies are required to investigate the dose range, efficacy, and safety.
The effect of a mixed cannabidiol and cannabidiolic acid based oil on client-owned dogs with atopic dermatitis. Melissa Loewinger, Joseph J. Wakshlag, Daniel Bowden, Jeanine Peters-Kennedy, Andrew Rosenberg. Vet. Derm. May 2022; doi: 10.1111/vde.13077. Quote: Background: Cannabidiol (CBD) and cannabidiolic acid (CBDA) are reported to have antinociceptive, immunomodulatory and anti-inflammatory actions. Objectives: To determine if CBD/CBDA is an effective therapy for canine atopic dermatitis (cAD). Animals: Thirty-two privately owned dogs with cAD. Materials and methods: Prospective, randomised, double-blinded, placebo-controlled study. Concurrent therapies were allowed if remained unchanged. Dogs were randomly assigned to receive either 2 mg/kg of an equal mix of CBD/CBDA (n = 17) or placebo for 4 weeks. On Day (D)0, D14 and D28, Canine Atopic Dermatitis Extent and Severity Index, 4th iteration (CADESI-04) and pruritus Visual Analog Scale (pVAS) scores were determined by investigators and owners, respectively. Complete blood count, serum biochemistry profiles and cytokine bioassays were performed on serum collected on D0 and D28. Results: Results of this study indicated that CBD/CBDA does not affect lesion severity yet does have a positive effect on pruritus as an adjunct therapy in some dogs with cAD. ...There was no significant difference in CADESI-04 from D0 to D14 or D28 in either group. pVAS scores were significantly lower for the treatment group at D14and D28 and a significant change in pVAS from baseline was seen at D14 and not D28 between groups. There was no significant difference in serum levels of interleukin (IL)-6, IL-8, monocyte chemoattractant protein - 1, IL-31 or IL-34 between groups at D0 or D28. Elevated alkaline phosphatase was observed in four of 17 treatment group dogs. Conclusions and clinical relevance: CBD/CBDA as an adjunct therapy decreased pruritus, and not skin lesions associated with cAD in dogs.
Pilot evaluation of a single oral fecal microbiota transplantation for canine atopic dermatitis. Koji Sugita, Ayaka Shima, Kaho Takahashi, Genki Ishihara, Koji Kawano, Keitaro Ohmori. Nature Sci. Rpts. May 2023; doi: 10.1038/s41598-023-35565-y. Quote: The gut microbiota has been suggested to be involved in the pathogenesis of canine atopic dermatitis (cAD). However, the gut microbiota has not been well characterized in dogs with atopic dermatitis (AD). In addition, the efficacy of fecal microbiota transplantation (FMT) in dogs with AD remains unclear. This research, therefore, aimed to characterize the gut microbiota of dogs with AD and conduct pilot evaluation of the efficacy of a single oral FMT on clinical signs and the gut microbiota of dogs with AD. For these purposes, we used 12 dogs [including 1 cavalier King Charles spaniel (CKCS), #8] with AD and 20 healthy dogs [including 2 CKCS]. The 16S rRNA analysis of the fecal microbiota revealed significant differences between 12 dogs with AD and 20 healthy dogs. Next, a single oral FMT was performed in 12 dogs with AD as a single-arm, open-label clinical trial for 56 days. ... Oral FMT was performed according to a procedure reported previously. In brief, immediately after collection of naturally excreted feces from the donor dogs, they were mixed with tap water. The fecal solution was filtered twice through a medical gauze pad, and then administered orally to dogs with AD using a syringe. ... A single oral FMT significantly decreased Canine Atopic Dermatitis Extent and Severity Index (CADESI)-04 scores from day 0 (median score, 16.5) to day 56 (8) and Pruritus Visual Analog Scale (PVAS) scores from days 0 (median score, 3) to day 56 (1). Furthermore, a single oral FMT changed the composition of the fecal microbiota of dogs with AD at the phylum and genus levels. The number of common amplicon sequence variants in the fecal microbiota between donor dogs and dogs with AD was positively correlated with CADESI-04 and PVAS reduction ratios 56 days after FMT. Our findings suggest that the gut microbiota plays a pivotal role in the pathogenesis of cAD, and that oral FMT could be a new therapeutic approach targeting the gut microbiota in cAD.
Oclacitinib 10 years later: lessons learned and directions for the future. Rosanna Marsella, Katherine Doerr, Andrea Gonzales, Wayne Rosenkrantz, Jennifer Schissler, Amelia White. JAVMA. June 2023; doi:10.2460/javma.22.12.0570. Quote: Oclacitinib was approved in the United States 10 years ago for the management of atopic dermatitis (AD) and allergic skin disease in dogs. Many studies and case reports have been published in the past 10 years on the efficacy and safety of this medication, both at labeled doses to treat allergic dogs and off label to treat other diseases and given to other species. Concerns and confusion have occurred for both clinicians and owners regarding the long-term safety of this drug. The purpose of this review is to present the current knowledge on the efficacy, speed of action, effects on the immune system, and clinical safety of oclacitinib, based on evidence and published literature. We also aim to summarize the lessons learned in the past 10 years and to propose directions for the future. ... We have learned about the safety, efficacy, and speed of action of oclacitinib compared to glucocorticoids. Instinctively we had assumed that injectable glucocorticoids would be faster than an oral medication, but the current evidence proves the opposite. ... While initially oclacitinib was considered a quick drug to stop itch, we now realize how blocking the signaling of so many cytokines involved in allergic inflammation affects a cascade of events that affect inflammation and not just pruritus. Yet, no study has specifically addressed this topic in a controlled fashion. Another question is whether oclacitinib could be of help for stenotic ear canals in allergic patients, a presentation for which the majority of dermatologists rely on glucocorticoids to decrease the swelling and inflammation. ... As the effect of oclacitinib on the various JAKs is concentration dependent and an issue of threshold, frequency of administration besides dose is important. Most case reports on the use of oclacitinib for autoimmune cases required twice-daily administration for extended periods of time to keep the diseases into remission highlighting the ability to immunosuppress by giving the medication more frequently and selecting the high end of the approved dose. As clinicians, we need to continue to be observant to provide the best care for our patients to maximize benefits and minimize unwanted adverse effects. Oclacitinib has proven to be a great tool in our armamentarium and has opened countless opportunities for an alternative option to the use of glucocorticoids.
Dermatological evaluation in dogs with atopic dermatitis treated with full-spectrum high cannabidiol oil: a pre study part 1. Carollina Mariga1, Ana Lűcia Souza Silva Mateus, Ângela Isabel dos Santos Dullius, Ana Paula da Silva, Mariana Martins Flores, Andrě Vasconcelos Soares, Erik Amazonas, Saulo Tadeu Lemos Pinto Filho. Front. Vet. Sci. October 2023; doi: 10.3389/fvets.2023.1285384. Quote: Introduction: Dermatological consultations represent a great part of the small animal medical clinic routine. Canine atopic dermatitis (CAD) is a common skin disease that affects a significant amount of dogs, making it a relevant consideration in clinical practice. The role of the endocannabinoid system on skin homeostasis has been described and its deregulation contributes to dermatopathies. Its function in specialized skin cells reveals an expressive therapeutic potential. Due to the difficulties and the growing scientific evidence of the therapeutic benefits of cannabis on animals, this work aimed to evaluate the anti-inflammatory effects of cannabis-derived oil in the treatment of CAD. Methods: Fourteen canines [none were cavaliers] diagnosed with CAD were divided into two groups: T: full spectrum high cannabidiol (CBD) cannabis oil, 2,5 mg/kg; and C: control group (treated with olive oil alone). The effectiveness was evaluated based on the degree of pruritus, dermatological evaluation (CADESI-4) and histopathological evaluation of the skin including mast cell count. Results: Despite the theoretical basis, there were no significant results obtained between the compared treatments. Discussion: Thus, it can be concluded that although full spectrum high cannabinoids therapy presents a promising approach to immunological diseases, further research is required in order to establish the actual effective cannabinoid ratio within the myriad possible combinations and for multi-target therapy of CAD.
Advances in Treatments for Canine Atopic Dermatitis. Cassie Donnell, Skyler Moore. Today's Vet. Pract. May 2024. Quote: Canine atopic dermatitis (AD) is a common allergic skin disease characterized by chronic inflammation, pruritus, and recurrent skin infections. The treatment of canine AD involves a multifaceted approach, including management of acute flares, chronic suppression of inflammation, restoration of the skin barrier, and allergen desensitization. In 2016, lokivetmab was the first monoclonal antibody approved for the treatment of canine AD. Lokivetmab offers a targeted approach for AD-associated pruritus in dogs and can serve as a useful therapy in both acute and chronic management. With its favorable side effect profile and efficacy, lokivetmab is a valuable addition for the management of canine AD. Furthermore, with the new approval of alternative dosage forms of oclacitinib and cyclosporine, as well as the exploration of alternative dosing regimens for oclacitinib, new advances in treatment of canine AD offer promising benefits to patient quality of life and client burden. However, despite arising therapies, classic mainstays of treatment, including corticosteroids, immunotherapy, and topical products, play an essential role in the multimodal management of canine AD. Take-Home Points: Lokivetmab is an effective agent in treating canine atopic dermatitis. Due to its rapid onset of effect and extended duration of action, it has become a popular agent for both the treatment of acute flares and chronic management. Lokivetmab’s mechanism of action is neutralization of interleukin-31. The most common adverse effects include injection-site pain, vomiting, diarrhea, anorexia, and lethargy. Development of antidrug antibodies may occur. There are no reported drug interactions. Alternate and/or concurrent treatment options include allergen-specific immunotherapy, oclacitinib, modified cyclosporine, and oral glucocorticoids. New formulations of oclacitinib (chewable tablet) and cyclosporine (generic solution) have been approved and may reduce client burden. Overall, canine atopic dermatitis is a complex disease that typically requires a multimodal approach to treatment in order to address the pathophysiology of the disease and provide control of clinical signs.
A placebo-controlled, double-blind study evaluating the effect of orally administered polyunsaturated fatty acids on the oclacitinib dose for atopic dogs. Laura Schäfer, Nina Thom. Ve. Derm. March 2024; doi: 10.1111/vde.13246. Quote: Background: Supplementation of polyunsaturated fatty acids (PUFA) ena- bles dose reduction of prednisolone and ciclosporin in canine atopic derma- titis (cAD). Objective: To determine if oral administration of PUFA reduces the dose of oclacitinib in cAD. ... The primary objective of this study was to determine if supplementation with PUFA reduces the dose of oclacitinib needed to control pruritus in dogs with AD over 16 weeks. Secondary objectives were to evaluate the effect of oral administration of PUFA on pruritus, lesion scores, QoL and quality-of- coat (QoC) in dogs with cAD. ... Animals: Twenty-two client- owned dogs with cAD receiving oclacitinib. Materials and Methods: Dogs received a fish oil product (PUFA) or paraffin oil (placebo) for 16 weeks. ... The study product was a fish oil containing 180 mg/ mL eicosapentaenoic acid (EPA) and 117 mg/mL docosahexaenoic acid (DHA; Omega-3 Support; WDT). The ratio of omega fatty acids was: omega-3: omega-6: omega-9 = 8.7:1.0:4.0. ... Owners adjusted the oclacitinib dose according to daily pruritus assessments. On Day (D)0, D56 and D112, Canine Atopic Dermatitis Extent and Severity Index, fourth iteration (CADESI- 04), pruritus Visual Analog Scale (PVAS), quality- of- life score (QoL), Global Assessment (GA), quality- of- coat (QoC) and adverse events were recorded. Results: Mean daily oclacitinib dose was significantly reduced in the PUFA group from 0.51 ± 0.20 mg/kg/24 h (D0) to 0.19 ± 0.14 mg/kg/24 h (D85–112; p < 0.00001) and not in the placebo group (D0: 0.70 ± 0.33 mg/kg/24 h; D85– 112: 0.53 ± 0.35 mg/kg/24 h, p = 0.5422). CADESI- 04 did not change over time or differ between groups. PVAS was significantly lower in the PUFA group (2.8 ± 1.5) compared to placebo (4.2 ± 1.6) at D112 (p = 0.0375). QoL and QoC improved only in the PUFA group (QoL: D0: 20 ± 7, D112: 12 ± 5, p = 0.0057; QoC: D0: 0 ± 0.5, D112: 1 ± 0.5, p = 0.0410). GA on D112 was higher in the PUFA group (p = 0.008). No adverse events were observed. Conclusion: Oral supplementation of PUFA allowed dose reduction of oclacitinib and improved PVAS, QoL, QoC and GA. The use of PUFA is recommended and was safe in the atopic study dogs receiving oclacitinib.
Evaluation of the efficacy and Safety of Palmitoylethanolamide (PEA) combination in managing dermatitis in dogs. Harsh J Shah, Jacky K. Pariyani, Kalyani V. Shinde, Bhakti A. Dave, Priyal B. Dakhore. Int'l j. Vet. Sci. & Anim. Husb. May 2025; doi: 10.22271/veterinary.2025.v10.i5d.2261. Quote: Dermatitis is a common inflammatory skin condition in dogs, caused by allergies, infections, or autoimmune responses, leading to significant discomfort and reduced quality of life (QoL). This study evaluated the effectiveness and safety of Palmitoylethanolamide (PEA) combination-PEA 300mg + Daidzein 50mg + Genistein 4mg -in 18 [Labrador retriever] dogs suffering from dermatitis. Dogs received PEA Combination twice daily for 28 days and were assessed on day 0 (baseline), 07, 14, 21 and 28 (End of study). Key evaluations included Canine Atopic Dermatitis Extent and Severity Index-4 (CADESI-4) and owner-reported QoL. CADESI-4 reduced significantly from 52.27±5.51 to 3.83±2.89 (p<0.001). QoL score significantly improved from 13.33±2.11 to 0.61±0.97 (p<0.001), while family concern scores improved from 5.55±1.33 to 0.22±0.42. Two cases of vomiting were reported as adverse events. The study concluded that PEA combination significantly reduced dermatitis and improved QoL in dogs, demonstrating safety and tolerability with no major adverse event.
RETURN TO TOP
Cyclosporine-induced dermatosis:
Cyclosporine-induced psoriasiform-lichenoid dermatosis in four dogs: Successful treatment with antibiotics and cyclosporine dosage reduction. Junko Ike, Ryosuke Ueda, Takeshi Mukosaka, Maiko Sekiguchi, Toshiroh Iwasaki. Vet. Rec. August 2024; doi: 10.1002/vrc2.984. Quote: Four dogs received cyclosporine at dosages of 8.6–17.5 mg/kg/day for 7–10 months to treat immune-mediated diseases. These dogs developed multiple, well-circumscribed lichenoid plaques with erythema and hyperpigmentation; additionally, thick scales appeared around the eyes, mouth and inside the auricles, and spread to almost the entire body. ... Case 1: A 7-year-old, neutered, male Cavalier King Charles spaniel exhibited chronic eczema with hyperpigmentation and hair loss around the eyes, mouth and abdomen 2 months ago. The dog had been orally administered cyclosporine (17.5 mg/kg/day) and prednisolone for polyarthritis for 7 months, but the prednisolone had been discontinued for 5 days due to the onset of dermatitis. The dog had multiple, well-circumscribed lichenoid plaques, hyperpigmentation, thick scales, erythema, papules, crusts and hair loss over the entire body [including around the eyes, around the mouth, and the back, chest, and abdomen]. ... On the basis of histopathological examination and medication history, the four dogs were diagnosed with cyclosporin-induced psoriasiform-lichenoid dermatosis. Three of the four dogs [including Case 1] exhibited marked improvement or disappearance of the skin lesions after systemic administration of antibiotics and reduction of the cyclosporine dosage; in the other dog, the lesions disappeared after systemic administration of antibiotics. ... Case 1: The dog received amoxicillin administered systemically (17.5 mg/kg twice daily) for 1 week, and was washed with shampoo containing salicylic acid (Keratolux, Virbac) and moisturiser (oats dermal calm, Zenoaq), with no obvious improvement. The dosage of cyclosporine was then reduced from 17.5 to 8.8 mg/kg/day. Three weeks later, hair growth occurred around the mouth and trunk, and 8 weeks after reduction of cyclosporin, the lichenoid plaques, scales and hyperpigmentation had almost disappeared. ... Case 1 died 3.5 months later of unrelated cause, but had no recurrence during that time. ... Cyclosporine-induced psoriasiform-lichenoid dermatosis is believed to be multifactorial, involving the immune system and resident cocci on the skin.
RETURN TO TOP
Dermoid sinus:
Diagnosis and surgical management of a type IVb dermoid sinus in a Cavalier King Charles Spaniel. Cecilia-Gabriella Danciu, Chiara Briola, Veerle Volckaert, Daniella McCready, Rachel Pittaway, Sue Fitzmaurice. Vet. Rec. December 2023; doi: 10.1002/vrc2.786. Quote: A 6-year-old, male, neutered Cavalier King Charles Spaniel dog was referred with a 4- year history of an intermittently draining fistula on the midline of the frontal bones of the skull. Magnetic resonance imaging and computed tomography scan of the head demonstrated an extra-axial mass in the midline between the frontal lobes, contacting themeninges and extending rostrally through a defect in the frontal bones. The mass was surgically excised via a frontal craniotomy. Histopathology of the mass demonstrated stratified squamous and keratinising epithelium with adnexal structures, consistent with the diagnosis of a dermoid sinus. Previous reports have documented dermoid sinuses in the nasal region in dogs and catswith intracranial extension. This case report documents a dermoid sinus in the frontal region with intracranial extension in a dog, confirmed by advanced diagnostic imaging, histopathology, and successfully treated surgically.
RETURN TO TOP
Malassezia dermatitis:
Malassezia dermatitis in the dog: a retrospective histopathological and immunopathological study of 86 cases (1990-95). Elizabeth A. Mauldin, Danny W. Scott, William H. Miller, Jr., Christina A. Smith. Vet. Derm. September 1997;8(3):191-202. Quote: In our study, West Highland White Terriers, English Setters, Shih Tzus, Basset Hounds and American Cocker Spaniels were at increased risk for developing Malassezia dermatitis. ... Other breeds reported to be at increased risk [for developing Malassezia dermatitis] include ... Cavalier King Charles spaniels... .
Malassezia Dermatitis. Jennifer L. Matousek, Karen L. Campbell. Compendium. March 2002;24(3):224-232. Quote: Other breeds of dogs predisposed to Malassezia dermatitis and otitis include the ... cavalier King Charles spaniel ... . Breed prevalence may suggest an inherited predilection for Malassezia dermatitis or may be a reflection of a hereditary predisposition for underlying disorders (e.g., hypersensitivity).
The method of application and short term results of tympanostomy tubes for the treatment of primary secretory otitis media in three Cavalier King Charles Spaniel dogs. Corfield GS, Burrows AK, Imani P, Bryden SL. Aust Vet J. March 2008;86(3):88-94. Quote: Case 1: A 4-year-old desexed female Cavalier King Charles Spaniel was presented to the Murdoch University Veterinary Hospital with a history of chronic, non-seasonal, bilateral otitis externa of approximately 2 years duration in conjunction with a recent onset of pedal and facial pruritus. ... Cytological examination of otic exudates retrieved from both ears ... revealed Malassezia organisms ... predominantly adhering to corneocytes. Cytological examination of tape strip samples collected from the interdigital and interpad region of all four feet, examined as above, revealed cocci and Malassezia organisms 1 to 3/OIF. A provisional diagnosis of bilateral Malassezia otitis externa and bacterial and Malassezia pododermatitis secondary to underlying hypersensitivity dermatitis (atopic dermatitis or adverse food reaction) was made. ... Case 3: A 6-year-old desexed female Cavalier King Charles Spaniel presented for assessment of presumed bilateral deafness, apparent for the previous 6 months. ... Cytological examination of samples of otic discharge taken from the left and right horizontal ear canals revealed Malassezia 4 to 6/OIF, and 6 to 8/OIF respectively. ... Oral ketoconazole 5 mg/kg every 12 hours was prescribed for 4 weeks to treat the Malassezia infection. ... In addition the first dog received topical betamethasone otic drops, a topical medicated shampoo and a systemic antifungal agent for the treatment of Malassezia otitis externa and bacterial and Malassezia pododermatitis. Dog 3 received a systemic antifungal agent for treatment of bilateral Malassezia otitis externa.
RETURN TO TOP
Mange:
Cheyletiella dermatitis in humans, dogs and cats.
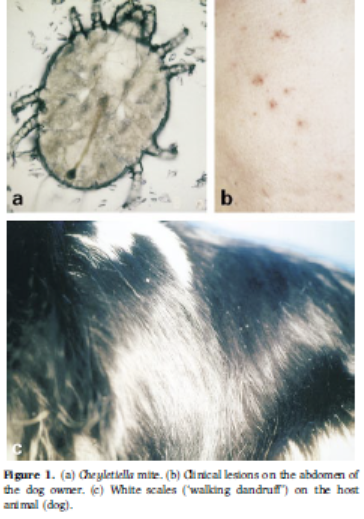 R. Wagner
N. Stallmeister. Brit. J. Dermatology. November
2000;143(5):1110-1112. Quote: In animals, Cheyletiella dermatitis
(walking dandruff) is usually a highly contagious but mild,
non-suppurative mite-induced dermatitis produced by Cheyletiella
spp. These parasites live on the skin of cats, dogs, rabbits and
humans. The non-burrowing mites live in the keratin layer of the
epidermis and feed on surface debris and tissue fluids. Their ova
are smaller than louse nits and are attached to hairs by fine
fibrillar strands. The egg-larval-nymphal-adult stages are completed
within 21 days on one host. Adult females may live free of their
host for up to 10 days. Eggs that are shed with the animals' hair
into the environment are important sources of reinfestation. Humans
may serve as an accidental or transitory host. The prevalence may be
underestimated because of false-negative samples. ... Case 3. A
7-year-old female Cavalier King Charles spaniel was brought to the
[Vienna, Austria] Dermatology Service with a 2-month history of
itch. One month after onset of the dog's pruritus [itching], the
owner's abdomen (Fig. 1b [right]) and legs were covered with pruritic red
papules. Examination of the dog revealed a few white scales over the
dorsum [back] (Fig. 1c). The skin looked normal. Acetate samples
from scales revealed many living Cheyletiella mites and eggs. For
the dog, dips with phoxim three times weekly were prescribed. After
two baths the owner reported decreased pruritus in the dog; in
addition, the owner's lesions and pruritus were decreased. After
three baths the dog was still a little itchy. Additional therapy was
given with moxidectin, two treatments 8 days apart. Lesions and
pruritus disappeared in both the dog and the owner. There are
numerous reports of skin disease due to Cheyletiella spp. in humans.
The mites are highly contagious, and in households with infested
animals 20% of pet owners are also infected.
R. Wagner
N. Stallmeister. Brit. J. Dermatology. November
2000;143(5):1110-1112. Quote: In animals, Cheyletiella dermatitis
(walking dandruff) is usually a highly contagious but mild,
non-suppurative mite-induced dermatitis produced by Cheyletiella
spp. These parasites live on the skin of cats, dogs, rabbits and
humans. The non-burrowing mites live in the keratin layer of the
epidermis and feed on surface debris and tissue fluids. Their ova
are smaller than louse nits and are attached to hairs by fine
fibrillar strands. The egg-larval-nymphal-adult stages are completed
within 21 days on one host. Adult females may live free of their
host for up to 10 days. Eggs that are shed with the animals' hair
into the environment are important sources of reinfestation. Humans
may serve as an accidental or transitory host. The prevalence may be
underestimated because of false-negative samples. ... Case 3. A
7-year-old female Cavalier King Charles spaniel was brought to the
[Vienna, Austria] Dermatology Service with a 2-month history of
itch. One month after onset of the dog's pruritus [itching], the
owner's abdomen (Fig. 1b [right]) and legs were covered with pruritic red
papules. Examination of the dog revealed a few white scales over the
dorsum [back] (Fig. 1c). The skin looked normal. Acetate samples
from scales revealed many living Cheyletiella mites and eggs. For
the dog, dips with phoxim three times weekly were prescribed. After
two baths the owner reported decreased pruritus in the dog; in
addition, the owner's lesions and pruritus were decreased. After
three baths the dog was still a little itchy. Additional therapy was
given with moxidectin, two treatments 8 days apart. Lesions and
pruritus disappeared in both the dog and the owner. There are
numerous reports of skin disease due to Cheyletiella spp. in humans.
The mites are highly contagious, and in households with infested
animals 20% of pet owners are also infected.
Efficacy of selamectin in the treatment of canine cheyletiellosis. R. S. Mueller, S. V. Bettenay. Vet. Rec. December 2002; doi:10.1136/vr.151.25.773. Quote: This short communication describes the efficacy of selamectin in the treatment of cheyletiellosis in two multidog households. Three breeding colonies in two households were treated. One household (household 1) consisted of nine cavalier King Charles spaniels. The referring veterinarian had identified Cheyletiella mites in superficial skin scrapings from one dog. This dog had been pruritic for several weeks, as had its owner. ... All of the dogs were treated by one of the authors (R. M.) with selamectin every other week at the recommended dose of 6 to 12 mg/kg for a total of four treatments. After spreading the hair between each dog's shoulder blades, the selamectin was applied as a spot-on. In household 1, which had fewer dogs, methoprene was used in the environment immediately after the first treatment of the dogs. ... Superficial skin scrapings, tape preparations and hair and scale samples obtained with a flea comb from each of the dogs, were evaluated microscopically immediately before the first and after the last treatments. ... In household 1, four dogs showed mild to moderate scaling of the trunk, and one dog and the owner were pruritic. Before therapy with selamectin, C yasguri mites were identified in a number of dogs with the various diagnostic tests used. Skin scrapings, tape preparations and hair plucks of all dogs were negative after four treatments with selamectin. The pruritus subsided in all dogs and the affected owner. ... On the basis of the findings of this study, selamectin is a safe and effective means of treating C yasguri in multidog households.
RETURN TO TOP
Necrolytic dermatitis:
Treatment of Superficial Necrolytic Dermatitis with Copper Chelationina Dog with Copper-Associated Hepatitis. Cindy Talbot, Shawn Kearns, Pamela J. Mouser. J. Am. Hosp. Assn. January 2023; doi: 10.5326/JAAHA-MS-7217. Quote: A 7 year old castrated male Cavalier King Charles spaniel presented for evaluation of liver enzyme elevations. Abdominal ultrasound revealed a small liver with mixed echogenicity, small hypoechoic nodules, and an irregular surface. Histologic examination and copper quantification of the liver obtained by laparoscopy diagnosed copper-associated hepatitis. One month later the dog developed hyperkeratosis of all four foot pads and ulcerations of feet, legs, and rectum. Punch biopsies confirmed superficial necrolytic dermatitis. After a total of 2 mo of chelation with no changes to medications, skin lesions began to improve, continuing over the following 6 wk to almost complete resolution. At this point the skin lesions returned and had minimal response to four amino acids infusions. The dog was switched from penicillamine to trientine. Zinc acetate was initiated 6 wk after the switch to trientine, and skin improvement was noted soon thereafter. At the time of death, skin lesions were improving and the dog was clinically comfortable. Copper-associated hepatitis should be considered as a possible etiology for superficial necrolytic dermatitis. Treatment of superficial necrolytic dermatitis is often unrewarding, and copper chelation, when copper-associated hepatitis has been confirmed, represents another therapeutic option.
RETURN TO TOP
Pemphigus foliaceus:
Polysulfated Glycosaminoglycan as a Novel, Adjunctive Therapy for
Pemphigus Foliaceus in Three Dogs. Andrew Simpson, Rod
Rosychuck, Jennifer Schissler, Clarissa Souza. J. Am. Anim. Hosp.
Assn. September 2019; doi: 10.5326/JAAHA-MS-6750.
 Quote:
Three dogs who were presented with cutaneous lesions and had
histopathologic findings consistent with pemphigus foliaceus were
treated with injectable polysulfated glycosaminoglycan as an
adjunctive to systemic immune-modulatory therapy. ... Case 1: A 9 yr
old, 12.6 kg castrated male Cavalier King Charles spaniel
was presented with a 6 mo history of pruritus and crusting.
Multifocal crusts and moderate hyperkeratosis affected the paw pad
margins. There was severe crusting on all claw folds. A
well-demarcated erythematous plaque with mild peripheral crusting
involved the prepuce and skin within a 2 cm radius around the
prepuce. There was moderate crusting of the scrotum. Severe
symmetric crusting and erythema affected the perianal region,
periocular region, medial aspects of both pinnae, and the lateral
muzzle. Histopathology of the skin obtained via punch biopsies
confirmed a diagnosis of PF [pemphigus foliaceus]. [See
photograph.] ... These patients were not adequately controlled
with oral glucocorticoids in conjunction with cyclosporine,
azathioprine, and/or mycophenolate. Polysulfated glycosaminoglycan
contributed to induction of remission and reduced glucocorticoid
doses in all dogs.
Quote:
Three dogs who were presented with cutaneous lesions and had
histopathologic findings consistent with pemphigus foliaceus were
treated with injectable polysulfated glycosaminoglycan as an
adjunctive to systemic immune-modulatory therapy. ... Case 1: A 9 yr
old, 12.6 kg castrated male Cavalier King Charles spaniel
was presented with a 6 mo history of pruritus and crusting.
Multifocal crusts and moderate hyperkeratosis affected the paw pad
margins. There was severe crusting on all claw folds. A
well-demarcated erythematous plaque with mild peripheral crusting
involved the prepuce and skin within a 2 cm radius around the
prepuce. There was moderate crusting of the scrotum. Severe
symmetric crusting and erythema affected the perianal region,
periocular region, medial aspects of both pinnae, and the lateral
muzzle. Histopathology of the skin obtained via punch biopsies
confirmed a diagnosis of PF [pemphigus foliaceus]. [See
photograph.] ... These patients were not adequately controlled
with oral glucocorticoids in conjunction with cyclosporine,
azathioprine, and/or mycophenolate. Polysulfated glycosaminoglycan
contributed to induction of remission and reduced glucocorticoid
doses in all dogs.
RETURN TO TOP
Piebaldism:
 Analogs
of human genetic skin disease in domesticated animals.
Justin Finch, Stephanie Abrams, Amy Finch. Int'l J. Women's Derm.
March 2017. Quote: Genetic skin diseases encompass a vast, complex,
and ever expanding field. Recognition of the features of these
diseases is important to ascertain a correct diagnosis, initiate
treatment, consider genetic counseling, and refer patients to
specialists when the disease may impact other areas. Because
genodermatoses may presentwith a vast array of features, it can be
bewildering to memorize them. This manuscript will explain and
depict some genetic skin diseases that occur in both humans and
domestic animals and offer a connection and memorization aid for
physicians. In addition,we will explore howanimal diseases serve as
a model to uncover the mechanisms of human disease. The genetic skin
diseases we will review are pigmentary mosaicism, piebaldism,
albinism, Griscelli syndrome, ectodermal dysplasias, Waardenburg
syndrome, and mucinosis in both humans and domesticated animals. ...
Cavalier King Charles Spaniel dog demonstrates
axial depigmentation. (Right)
Analogs
of human genetic skin disease in domesticated animals.
Justin Finch, Stephanie Abrams, Amy Finch. Int'l J. Women's Derm.
March 2017. Quote: Genetic skin diseases encompass a vast, complex,
and ever expanding field. Recognition of the features of these
diseases is important to ascertain a correct diagnosis, initiate
treatment, consider genetic counseling, and refer patients to
specialists when the disease may impact other areas. Because
genodermatoses may presentwith a vast array of features, it can be
bewildering to memorize them. This manuscript will explain and
depict some genetic skin diseases that occur in both humans and
domestic animals and offer a connection and memorization aid for
physicians. In addition,we will explore howanimal diseases serve as
a model to uncover the mechanisms of human disease. The genetic skin
diseases we will review are pigmentary mosaicism, piebaldism,
albinism, Griscelli syndrome, ectodermal dysplasias, Waardenburg
syndrome, and mucinosis in both humans and domesticated animals. ...
Cavalier King Charles Spaniel dog demonstrates
axial depigmentation. (Right)
RETURN TO TOP
Staphylococcus intermedius:
Diversity and stability of the Staphylococcus intermedius flora in three bitches and their puppies. L. E. M. Saijonmaa-Koulumies, V. Myllys, D. H. Lloyd. Epidemiol. Infect. October 2003; doi: 10.1017/S0950268803008938. Quote: The study investigated the transfer and the stability of the S. intermedius flora in three bitches and their puppies. A total of 240 cutaneous and mucosal isolates of S. intermedius was collected from three healthy Cavalier King Charles spaniels and their puppies during the immediate prepartum period and after whelping, over a total of 15 weeks. The isolates were genotyped with random amplified polymeric DNA-polymerase chain reaction analysis (RAPD-PCR) using two primers. Seventeen different genotypes of S. intermedius were identified. One or two of the genotypes were dominant in each of the bitches and their puppies. The rest were isolated only once or twice from the bitches or their puppies. The study indicates that S. intermedius flora within each studied bitch mainly consisted of one or two dominating and persistent clones, which were transferred from the dam to her puppies immediately after birth.


CONNECT WITH US